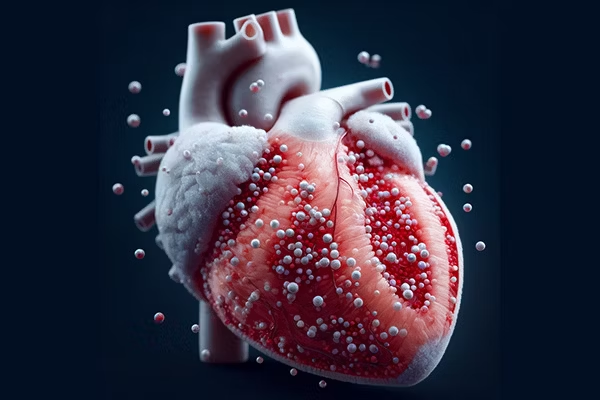
Custom Nanoparticles That Can Transport Drugs to the Heart
With a $2.07 million, four-year grant from the National Institutes of Health, Jianjun Guan, a materials scientist at Washington University in St. Louis’ McKelvey School of Engineering, and his team intend to encase a peptide that prevents fibrosis and a set of proteins that reduce inflammation inside deceptively disguised drug-delivering smart nanoparticles.
According to the Centers for Disease Control & Prevention, a heart attack occurs in the United States every 40 seconds, and almost 300,000 of those victims do not require surgery to restore blood flow. It has been difficult to get drugs to the heart for these patients, who depend on them to lower inflammation and prevent the formation of scar tissue or fibrosis.
The nanoparticles would be administered intravenously into the bloodstream, going straight to the heart.
Current treatments target fibrosis and inflammation separately, but their efficacy in clinical studies has not been adequate. Anti-inflammatory drugs can impede the healing of the heart or fail to target inflammatory signals in the heart when administered at the appropriate time or place. Similarly, treatment for cardiac fibrosis usually solely addresses one of the pathways leading to fibrosis and does not block other pathways.
Guan’s team intends to investigate the secretome of M2 macrophages, or the proteins and cytokines produced by M2 macrophages, to minimize inflammation and promote tissue healing in cardiac therapy. Mohamed Zayed, MD, PhD, a professor of surgery, radiology, and molecular cell biology at the School of Medicine and biomedical engineering at McKelvey Engineering, is working with Guan on the study.
After a heart attack, a dominated cell type in the inflammatory phase is a macrophage called M1, while at the anti-inflammatory phase is a macrophage named M2. If we can quickly deliver the secretome made by the M2 macrophage after a heart attack, it can rapidly transition the inflammatory phase to the anti-inflammatory phase.
Jianjun Guan, Materials Scientist, McKelvey School of Engineering, Washington University in St. Louis
Researchers have attempted to treat cardiac fibrosis using TGFβ and antibodies but achieved minimal success.
Guan’s team has created a peptide-based inhibitor, abbreviated RPE, that inhibits TGFβ and other processes that cause fibrosis. According to preliminary research, RPE drastically reduced the density of myofibroblasts, or cells present in scar tissue, following a heart attack.
Guan’s goal is to load a nanoparticle with two components—an M2 secretome and an RPE—and coat it with a blood platelet membrane so that the immune system sees it as part of the blood, he added. He will also immobilize a peptide particular to the injured area of the heart.
Guan added, “When we immobilize such a peptide on the nanoparticle, it forms a brush on the nanoparticle surface. This brush will recognize the injured area of the heart, go directly to it and gradually release the drugs.”
Guan’s team will also investigate the timing of the nanoparticles’ injection to determine whether there is a difference in efficacy. They will administer the drugs in a preclinical model one, three, and seven days after a heart attack to determine whether they have a therapeutic impact.
“Our final goal is that we make the nanoparticles available in a form that a patient could inject at home after a heart attack. We are also looking at a form that they could be inhaled into the lungs and go to the heart,” Guan concluded.
Source: https://wustl.edu/
